By Michael Schwartz, MD
The goal of personalizing cancer treatments by targeting molecular alterations in tumors has seen rapid advances in the past 20 years. Knowledge of the mechanisms associated with cancer initiation and progression has recently improved with the increasing use of molecular techniques, enabling identification of alterations in cancer cells and subsequent development of therapeutic agents targeting these alterations. Central to the drive for personalized medicine is the need to develop specific diagnostic tests that facilitate identification of patients who are most likely to respond to a given treatment. Such tests have been referred to as “companion diagnostics” (CDx), and can play an essential role in outcome prediction as well as therapy monitoring.
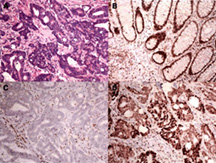
The lifetime risk for colorectal carcinoma (CRC) is about five percent in developed countries. New molecular testing guidelines are currently being developed. Per the draft guideline, all patients with CRC being considered for treatment with the EGFR inhibitors cetuximab and panitumumab should undergo extended RAS mutational testing to predict their response to the drugs. The draft guideline calls for extended mutational analysis that includes KRAS and NRAS codons 12 and 13 of exon 2, codons 59 and 61 of exon 3, and codons 117 and 146 of exon 4. Studies have shown that patients who had mutations in KRAS exons 2, 3 and 4 and in NRAS exon 2 and 3 do not benefit from anti-EGFR therapy and could suffer from those agents. The guidelines are expected to recommend BRAF V600 mutation analysis in conjunction with deficient DNA mismatch repair/microsatellite instability (dMMR/MSI) testing for patients with metastatic colorectal carcinoma, and dMMR/MSI testing in all patients for prognostic stratification and identification of Lynch syndrome. The final guideline should be published in the near future.
For CRCs, TNM stage remains the best predictor of survival after resection and the key determinant of patient management. Nevertheless, stage-independent variability in clinical outcome is sometimes observed and likely due to molecular heterogeneity. This is particularly important in early stage CRC where patients can be potentially cured by surgery alone, and only a proportion derive benefit from adjuvant chemotherapy. For these patients, identification of prognostic molecular markers to supplement conventional staging can change management and outcomes. For example, CRCs with dMMR and MSI have a better stage-adjusted survival compared to proficient MMR or microsatellite stable tumors. In addition, most studies indicate that patients with stage II dMMR CRCs do not benefit from 5FU based chemotherapy and can be treated by surgery alone.
A recent article (N Engl J Med 2016;374:211-222) identified a subgroup of patients with stage II colon cancer who appeared to benefit from adjuvant chemotherapy. In this study, those whose CRC lacked nuclear expression of CDX2 (a master regulator of intestinal development) by immunohistochemistry were associated with a lower rate of five-year disease-free survival than CDX2 positive tumors. Furthermore, the rate of five-year disease-free survival was higher among patients with stage II CDX2-negative tumors who were treated with adjuvant chemotherapy than among patients who were not treated with adjuvant chemotherapy.
Companion diagnostics are continuing to evolve in CRC, where they are becoming an essential tool for selecting the most appropriate personalized therapeutic treatment.
 Dr. Schwartz attended medical school at SUNY Upstate Medical University in Syracuse, NY and completed his residency in combined Anatomic and Clinical Pathology at the University of Pittsburgh Medical Center where he was Chief Resident and later a staff pathologist. He is a member of Peninsula Pathology Associates and works at Riverside Regional Medical Center in Newport News. ppapathology.com
Dr. Schwartz attended medical school at SUNY Upstate Medical University in Syracuse, NY and completed his residency in combined Anatomic and Clinical Pathology at the University of Pittsburgh Medical Center where he was Chief Resident and later a staff pathologist. He is a member of Peninsula Pathology Associates and works at Riverside Regional Medical Center in Newport News. ppapathology.com

