 By Alan L. Wagner, MD
By Alan L. Wagner, MD
You may wonder, what do Hampton Roads Physician’s article on hospital medicine and my specialty of retina vascular disease research and ocular oncology have to do with one another? As it turns out – a lot!
Twenty four percent of adult patients with known diabetes say that they had been hospitalized in the preceding year. The risk of hospitalization increases with age, how long the patient has had diabetes, and the nature and extent of any other sequelae of the disease. A patient with diabetes is three times more likely to be hospitalized than those who don’t have diabetes. If we look at all the people admitted to the hospital, 12 percent didn’t realize that they had diabetes, or unusually high blood sugars. These are the very patients who are at risk for blindness without warning from diabetes – and one of the reasons the job of the hospitalist is so vital.
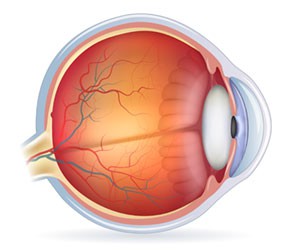
 Hospitalists see their patients more than once during the day, and may have more opportunity to observe the warning signs of diabetic eye disease – which remains the leading cause of blindness and disability in adults in the first world. However, in the outpatient setting, the silent and progressive damage to the retinal vasculature that is preventable can go unnoticed.
Hospitalists see their patients more than once during the day, and may have more opportunity to observe the warning signs of diabetic eye disease – which remains the leading cause of blindness and disability in adults in the first world. However, in the outpatient setting, the silent and progressive damage to the retinal vasculature that is preventable can go unnoticed.
The root cause of much of this physiologic mayhem comes from above normal blood sugars. Not “high” blood sugars, just above normal blood sugars! However, it’s really not the elevated blood sugar itself that does the damage. Higher than normal blood sugars cause the immune system to become abnormally and broadly activated, leading to inflammatory changes in the vascular endothelium. As inflammation increases, the endothelium of the eyes, brain, heart, nerves, and kidneys become targets, leading to thrombosis. For similar reasons, platelets become far more active and sticky, compounding the problem. In addition, the elevated blood sugars cause increases in multiple inflammatory pathway associated proteins/markers (interleukins, tumor necrosis factors, growth hormones, advanced glycated End products, etc.). We see the same sort of proteins and damage in patients with arthritis. However, this time it’s the blood vessels that are targeted for destruction.
Hospitalists and their teams can serve as a tremendous educational resource for patients and their families by explaining to them that it doesn’t take very high blood sugars to cause these changes that can lead to blindness. The landmark Diabetes Control and Complications Trial revealed that patients with normal blood sugars were able to reduce their risk of complications from diabetes by almost 50 percent. This is in line with what we already know about reducing the risk of diabetes associated coronary disease, renal disease, neuropathy, and strokes. In other words, we can show the patients and their families that there really is a big pay-off if they control their diabetes.
Hospitalists do so much good for patients while they’re in the hospital. I encourage our ambulatory care colleagues to also be proactive, by reminding their patients of the critical need to normalize blood sugars, get regular eye examinations, and seek consultation with an eye specialist – particularly if they have or show signs of developing diabetes. As a memory tool, feel free to use our practice’s take-home message for all of our at-risk patients: “Save your sight by feeding your eyes normal blood at a normal pressure!”
 Alan L. Wagner, MD, FACS founded the Wagner Macula & Retina Center in 1987. He completed medical school at Vanderbilt University School of Medicine, residency at EVMS and a fellowship at Weill Cornell University Medical Center. wagnerretina.com
Alan L. Wagner, MD, FACS founded the Wagner Macula & Retina Center in 1987. He completed medical school at Vanderbilt University School of Medicine, residency at EVMS and a fellowship at Weill Cornell University Medical Center. wagnerretina.com

