By Bradley Prestidge, MD, MS
Regional Medical Director for Radiation Oncology
Bon Secours Cancer Institute in Hampton Roads
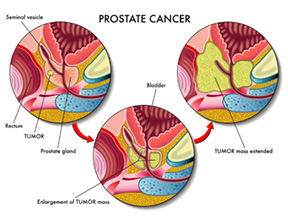
Men facing the diagnosis of prostate cancer have both surgical and non-surgical treatment options, depending on their stage of disease. If the cancer is believed not to have spread outside the prostate, they can undergo radical prostatectomy, removing the gland and some of the surrounding tissue, including the seminal vesicles.
Most often, there are also a number of non-surgical treatment options. Four of those options involve radiation therapies:
External Beam Radiation
Image guided intensity modulated radiation therapy (IMRT or IGMRT), is an effective external beam treatment using high doses of radiation to kill prostate cancer cells. It requires a brief daily (Monday through Friday) treatment for up to nine weeks.
Brachytherapy
Brachytherapy involves placing radioactive pellets inside an organ or tumor. There are two types of prostate brachytherapy: low dose rate (LDR) and high dose rate (HDR.)
 LDR brachytherapy, sometimes called “seed implants” or “permanent brachytherapy,” is an outpatient procedure for patients with cancer confined to the prostate, in which tiny radioactive seeds are permanently placed in the prostate. These seeds emit low levels of radiation for an extended period, and need not be removed after becoming inert. The patient leaves the procedure with only minor safety precautions.
LDR brachytherapy, sometimes called “seed implants” or “permanent brachytherapy,” is an outpatient procedure for patients with cancer confined to the prostate, in which tiny radioactive seeds are permanently placed in the prostate. These seeds emit low levels of radiation for an extended period, and need not be removed after becoming inert. The patient leaves the procedure with only minor safety precautions.
HDR brachytherapy is not offered at all radiation facilities. The concept is similar to LDR, but instead of implanting multiple permanent seeds, a single radioactive pellet is inserted robotically through a hollow catheter or needle placed in the prostate under general anesthesia. The exact position of the pellet in each needle and the number of seconds that the pellet dwells in each position is computer driven and the entire treatment takes from 5-10 minutes to deliver.
HDR prostate brachytherapy may be given as monotherapy, but is more commonly used in combination with external radiation as a “boost.” However, because of a growing interest in shorter, more hypo-fractionated radiation approaches, HDR brachytherapy for prostate cancer used as monotherapy is being more intensively studied. The Bon Secours Cancer Institute at DePaul is one of only eight sites in the country invited to participate in a national protocol to be implemented next year providing HDR brachytherapy in a single, stand alone treatment for early and intermediate risk prostate cancer.
Combination Therapy
Depending on the stage of prostate cancer, very often a combination of therapies is recommended – for example, five weeks of daily radiation with HDR brachytherapy as a boost, or five weeks of external radiation using LDR brachytherapy as the boost.
Stereotactic Beam Radiation Therapy
SBRT is a technologically sophisticated form of external beam radiation delivered with even greater precision and at a much higher dose per fraction than conventional external beam treatment. Multiple radiation beams, or arcs, are designed to enter the body through various angles, intersecting at the prostate. Instead of eight to nine weeks of individual daily treatments, only five are required, spread out over two weeks. It is non-invasive, does not require general anesthesia, and results in very high cancer control rates, comparable to surgery and the other non-surgical approaches described above. To date, the Bon Secours Cancer Institute at DePaul is the only facility offering this option to men in Hampton Roads.
 Dr. Prestidge earned his medical degree from Uniformed Services University of the Health Sciences in Bethesda, MD, and served an internship in internal medicine at David Grant USAF Medical Center at Travis Air Force Base in Fairfield, CA. He served as an active duty Air Force physician and consultant to the Surgeon General for 12 years. In addition, he completed a residency in radiation oncology at Stanford University Hospital in Stanford, CA. http://www.bonsecours.com
Dr. Prestidge earned his medical degree from Uniformed Services University of the Health Sciences in Bethesda, MD, and served an internship in internal medicine at David Grant USAF Medical Center at Travis Air Force Base in Fairfield, CA. He served as an active duty Air Force physician and consultant to the Surgeon General for 12 years. In addition, he completed a residency in radiation oncology at Stanford University Hospital in Stanford, CA. http://www.bonsecours.com

