Expanding practices to encompass total care
When Orthopaedic & Spine Center (OSC) was founded in 1990, the physicians had a very clear vision: they wanted to offer the best and most comprehensive orthopaedic treatment available to the patients who entrusted them with their care. And they wanted to create a patient-centered environment in which to provide that care.

That philosophy continues to drive the practice. “OSC is constantly growing in order to provide a better experience of patient care,” says Jeffrey R. Carlson, MD, who joined the practice in 1999 and currently serves as President and Practice Manager. “We’re always looking for ways to help patients by implementing new surgical techniques and supportive care.” And indeed, OSC has recently expanded its services to include new modalities and perspectives on caring for patients with orthopaedic problems and chronic pain, concentrating on both superior patient care and patient service.
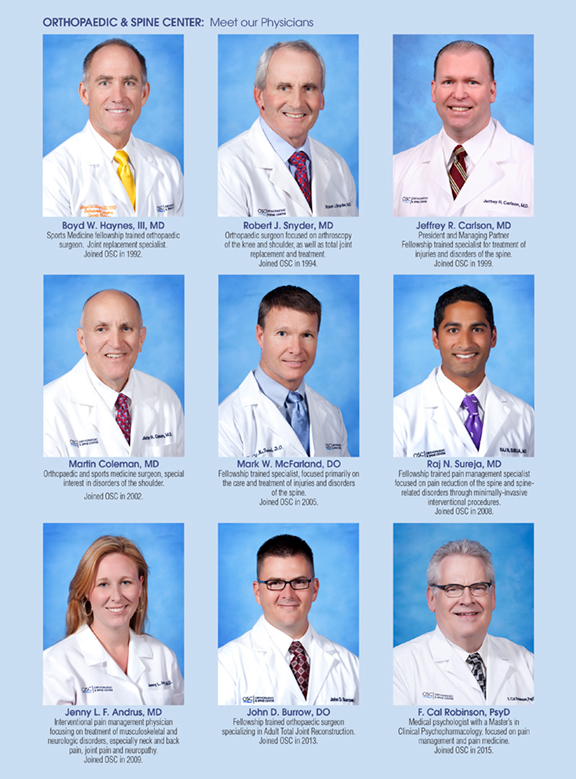
All OSC physicians – now numbering nine – are Board certified, and now include a medical psychologist with an extensive career in pain management and pain medicine. They have specialized training in every aspect of orthopaedic surgery and care, as well as chronic and interventional pain management. They are supported by expanded facilities featuring state-of-the-art technologies, complemented by an exceptional, highly trained and skilled staff.
New therapies with proven results.
The role of regenerative medicine.
“Far too often in the past,” says Raj N. Sureja, MD, “we’ve seen patients with conditions for which we’ve had limited treatment options, in both scope and efficacy. But once in a lifetime, real scientific advances are made that change everything for the patient and the physician.” Dr. Sureja and his colleagues at OSC believe Regenerative Medicine is that game-changer, in that it potentially allows physicians to heal patients in ways they could once only imagine.
Regenerative Medicine uses autologous or amniotic stem cells, which can develop into many types of cells through differentiation. As so many people in the United States are afflicted with arthritis and other musculoskeletal problems, such as back pain, rotator cuff tears, meniscal tears, etc., stem cell therapy is an excellent non-surgical therapy for patients who cannot have surgery or who choose not to.
“We’re already treating these patients with cortisone injections to control their pain,” Dr. Sureja says, “so from the patient’s perspective as well as the physician’s, Regenerative Medicine Therapy is no different. The difference lies in what we’re injecting. Instead of merely easing pain, we’re trying to repair or strengthen tissue that’s damaged or degenerating, using the body’s own stem cells or platelets and growth factors to minimize inflammation, which speeds recovery and can potentially heal tissue.”
Autologous cells cannot be rejected, and Dr. Sureja assures his patients that PRP is safe and effective, noting its approval by the NFL, MLB and the World Anti-Doping Association. In fact, many national and international sports leagues have adopted platelet rich plasma therapy as one of the first-line treatments of their injured athletes – including, among many others, Kobe Bryant and Hines Ward.
Prolotherapy – effective treatment for patients with chronic pain.
“Patients often present with a history of chronic pain, for which x-ray and MRI studies offer little or no explanation,” says Jenny L. F. Andrus, MD, who focuses on treating painful musculoskeletal and neurologic disorders. She routinely treats neck and back pain, joint pain and painful neuropathy. She often uses physical therapy, pain psychology and medications along with interventional procedures to target difficult chronic pain. She is a proponent of prolotherapy, a treatment of tissue with the injection of an irritant solution into a joint space, weakened ligament, or tendon insertion to relieve pain, which she has found effective in treating these patients.
“Most of the time, the injection is a high concentration of sugar water that brings in blood and causes inflammation, which causes the injury to heal,” Dr. Andrus says, acknowledging what has been seen to be a contradiction. “For years, we’ve been thinking inflammation is always bad, and giving patients an anti-inflammatory every time they have pain, when actually, people need a little inflammation to heal.”
Prolotherapy allows the body to do its own work. Instead of injecting a pharmacologic agent into the body, prolotherapy brings in the cells the body needs through its own blood supply, effectively enabling the body to heal itself. She’s especially excited about the positive benefit she’s seen for patients with chronic sacroiliac joint pain, and has begun working in collaboration with OSC’s Physical Therapy Center to establish an SI Joint program.
But, she cautions, there’s no magic number of treatments that are guaranteed to produce results for every patient. “Our patients usually begin to see some benefit after their third treatment,” she says. “But for those who are biomechanically set up to have a repetitive trauma-type injury, there may be the need to be on a maintenance regimen.” Not because the treatment wore off, she adds, but because those patients developed the injury again.
New techniques in spine surgery.
As one of OSC’s fellowship trained spine surgeons, Dr. Carlson is a proponent of outpatient spinal surgery procedures and techniques, including Less-Exposure Spine Surgery (LESS), which is minimally invasive and less traumatic for the patient. Along with his colleagues, he actively seeks new and advanced technologies as treatment options, carefully selecting those that will offer the best outcomes for his patients.
“The idea is that we try to limit surgical injury,” he explains, “so we use the same incision to get screws, rods, plates, bone graft, etc., into the surgical site that we are using to get the disc out – thus limiting the amount of surgical pain by decreasing the amount of soft tissue injury. In a cervical spine procedure, the procedure can be done with an incision no longer than an inch.”
He has successfully employed these techniques for lower back cases as well. “In the past, when we did a fusion, those incisions were three to four inches long, which resulted in significant pain requiring a hospital stay,” he says. “But we’re doing microdiscectomy incisions an inch, or an inch and a half long, and doing the fusion through that same incision.” His patients are up, getting their muscles moving so there’s much less spasming and far less pain. Their nerve pain is relieved, their bones are fixed and solid, and they’re getting back to their lives much more quickly. “It works,” Dr. Carlson says, “because we changed our thought process. We simply changed the angle at which we insert the hardware.”
Getting his patients up on their feet quickly and on their way home to recuperate is part of Dr. Carlson’s surgical plan. “Nobody wants to stay in the hospital,” he says. “Patients do better in their own environment, where they control when they sleep, what they eat and they’re surrounded by familiar comforts. These procedures take much less time, involve much less surgical injury and result in less post-operative pain.”
Outpatient Total Hip and Knee Replacement Program.
Joint replacement surgeries have been performed for more than 100 years, but it was only five years ago that they were done as outpatient procedures in Virginia, and OSC was at the forefront. In July 2010, OSC orthopaedic surgeon Boyd W. Haynes, III, MD performed the Commonwealth’s first outpatient knee replacement. Less than a month later, Mark W. McFarland, DO did the first outpatient total hip.
At the time, both surgeons remember, the orthopaedic community differed on whether these procedures were wise, fearing complications might arise that would require patients’ return to the hospital.
“The things that make the difference are better anesthetics, computer navigation and the most current surgical techniques,” says Dr. Haynes. “And our outpatient therapy program is a huge part of the success.”
The program always starts in Dr. Haynes’ office, with him talking to his patients, so he can make sure they have the right mindset, and that they understand what they are asking for. It always starts with education.
“We don’t want people in the hospital,” Dr. Haynes explains. “There are sick people in the hospital, and joint replacement patients aren’t sick.” But before they leave the operating room, his patients understand that therapy starts the same day as surgery – and therein lies the success of the program. All of the details of therapy have been painstakingly set in motion before the surgery. “I have protocols in place whereby if a patient’s surgery is on Wednesday, therapy starts that day and sets everything up to start in-home therapy on Thursday, just as it would if the patient stayed in the hospital,” Dr. Haynes says. “Even the hospital personnel are familiar with these protocols and make sure my patients are appropriate for discharge.” It’s a well-oiled system that works: in the five years since Dr. Haynes’ first outpatient surgery, none of these patients have had to come back to the hospital for admission.
Open MRI Center.
It had been clear for years that patients were experiencing anxiety and claustrophobia because of the lengthy time they were required to spend in a closed MRI unit. To address their discomfort, in 1992, soon after the technology came on the market, OSC purchased its first open MRI machine. In addition to providing a better experience for their patients, the physicians found the imaging equal to or better than the results of standard closed scanners.
In 2013, the practice invested in a state-of-the-art Hitachi Oasis 1.2T hospital grade MRI system, which sets the highest standard for patient-centric care. OSC has found that even the most challenging patients can be handled with confidence, and without compromising safety, performance or efficiency. A unique achievement in high-performance imaging, the Oasis open architecture features advanced magnet design, Zenith RF Technology and robust clinical capabilities to achieve high throughput diagnostic performance. “The big magnet defines the quality of the images,” Dr. Carlson says. “When we show these crisp pictures to the patients, they can see exactly what we’re talking about.”
The Physical Therapy Center.
Originally situated in 5,000 sq.ft. on the second floor of the main OSC building, the Physical Therapy department soon outgrew that space and in 2013, acquired its own dedicated building adjacent to OSC. To meet the needs of OSC’s growing patient population, four therapists – Tom Toothaker, DPT; Amanda Jetty, DPT and Junmei Pan, PT; and Clinic Director Rachel Tyler, DPT, CIMT – are now in place, supported by two licensed physical therapy assistants, Bill Richards, LPTA and Heather Cole, LPTA. Now operating in 8,000 sq.ft., the Physical Therapy Center features five private and five semi-private rooms, and open gym areas on either side of the building that accommodate cardiovascular equipment and more advanced equipment for high performing athletes.
A recent innovation of the Physical Therapy Center is dry needling, a technique for treating muscular pain, which has shown remarkable results. “The technique involves inserting a monofilament needle into a muscle in order to reset the muscle tissue and decrease trigger point activity,” says Tyler, who recently received her Doctorate in Physical Therapy. “Dry needling has been shown to be a remarkable adjunct to traditional manual and physical therapy techniques.” There are four therapists at the OSC Physical Therapy Center, who received this advanced training from KinetaCore®, a national organization that offers continuing education courses for manual therapists.
Dr. Tyler and her colleagues work in conjunction with all OSC physicians, caring for patients both before and after surgery, as well as non-surgical patients.
Healing body and mind.
Relieving orthopaedic pain is more complex than merely identifying and fixing the mechanisms causing the pain. “Even with patients who have a clear pathology, there’s a psychological component that is sometimes overlooked,” Dr. Andrus says. “We’re trying to focus on the whole person.”
In that vein, in August of 2015, OSC welcomed F. Cal Robinson, PsyD, MSCP, a Board certified medical psychologist with a Masters of Science in Clinical Psychopharmacology. Prior to joining OSC in August 2015, Dr. Robinson had an extensive career in pain management and pain medicine.
Dr. Robinson cites an Institute of Medicine report from 2011 evaluating the effectiveness of chronic pain treatment in the US, which showed that the interventional movement in pain management had resulted in many patients becoming passive recipients of opioid analgesic injections and procedures. “Very few interventions are more than a temporary fix,” Dr. Robinson says, “and as evidenced by that IOM report, the health community supports an integrated biopsychosocial approach to health and pain care. We want to see people shift to becoming more active participants in their own care.” He adds, “Orthopaedic and Spine Center has shown great wisdom in recognizing that we have to offer something other than pain reduction to these patients. We can help them from a treatment perspective by assisting them in finding ways to more effectively accept and live with pain.”
Acceptance and Commitment Therapies (ACT).
The American Psychological Association has endorsed ACT as a very effective therapy for chronic pain. “Within cognitive behavior science, the concepts of mindfulness, and acceptance and commitment therapies, have been emerging,” Dr. Robinson says. “The meaning and purpose of pain in one’s life have to be addressed. The idea is to learn to be present with the pain, finding one’s way toward accepting it: being intentionally mindful of the experience without reacting to it has been found to be incredibly helpful.”
People can change their mindsets. Rather than fighting and struggling with pain, he says, “We can teach them that they have the power to accept and deal with their pain. It’s not an easy shift, but it can be made.”
Always looking ahead.
The practice’s original vision – the most exceptional orthopaedic care in the most patient-welcoming atmosphere – is pursued by OSC every day, but never to the extent of resting on its considerable laurels. Every new modality will be tested, every new technique explored, every burgeoning therapy investigated – because OSC knows that with today’s medical advances, technology and innovation, there is no reason for anyone to put their lives on hold for orthopaedic or pain problems. OSC continues to demonstrate its longstanding commitment to putting patients first.
Orthopaedic & Spine Center
250 Nat Turner Boulevard, Newport News, VA 23606
757.596.1900
www.osc-ortho.com