Percutaneous fusion technique
is relieving SI pain in post-fusion patients.
By John W. Aldridge, MD, FAAOS
Every year in the United States, approximately 150,000 hip replacements are performed, and more than 350,000 knee replacements. By contrast, the number of spinal fusions done each year is a stunning 650,000, reflecting just how many Americans suffer from a seriously aching lower back. The overwhelming majority of these procedures are successful, reducing or substantially relieving pain and restoring the patients to comfortable, active lifestyles.
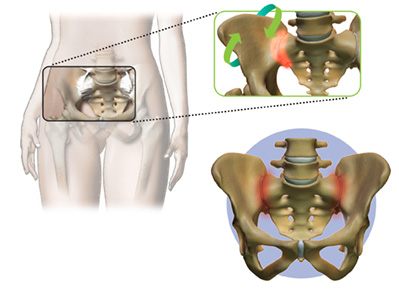 However, orthopaedic surgeons have long recognized – and recent studies have shown – that in some cases, fully a third of these patients experience significant sacroiliac joint problems following fusion. Additional studies have shown that the incidence of SI joint degeneration after lumbar fusion is 75 percent at five years post surgery. As arthritic patients, those who have suffered traumatic injuries, and even some pregnant women know well, SI joint pain can be debilitating, often resulting in discomfort equivalent to or even worse than that which brought them to our offices in the first place. It’s a commonplace but vexing problem for orthopaedic surgeons, because until recently we have had very little to offer them.
However, orthopaedic surgeons have long recognized – and recent studies have shown – that in some cases, fully a third of these patients experience significant sacroiliac joint problems following fusion. Additional studies have shown that the incidence of SI joint degeneration after lumbar fusion is 75 percent at five years post surgery. As arthritic patients, those who have suffered traumatic injuries, and even some pregnant women know well, SI joint pain can be debilitating, often resulting in discomfort equivalent to or even worse than that which brought them to our offices in the first place. It’s a commonplace but vexing problem for orthopaedic surgeons, because until recently we have had very little to offer them.
About the only surgical option required a gigantic dissection to get down into the SI joint to put plates and screws in, and the destruction that caused actually made people feel worse than the SI joint did. That’s why virtually no surgeons were offering it.
That’s changed within the last year or two with the introduction of the percutaneous fusion technique. It’s a simple but effective minimally invasive procedure that is substantially reducing and even eliminating the effects of SI pain, including in post-spinal fusion patients.
In the operating room, the patient is positioned face down on the table, under either general or spinal anesthesia, depending on size, weight and presentation. Using live imaging, the surgeon employs a specially designed system that prepares the bone to receive implants that will stabilize and fuse the SI joint. One of two devices, either screws or pegs, depending on the quality of the bone, is used. Generally, no larger than a one-inch incision in the lateral buttock is required to place the device into which the implants are threaded and placed across the SI joint and positioned before fusing them. There are normally three implants, but again, that can vary depending on the patient.
The procedure takes about an hour, is easily tolerated, and some patients can even go home right after the procedure, although most stay overnight. Patients use a walker for two or three weeks after the surgery, and they’re fully healed and out of pain after about six weeks.
The procedure has been a real godsend for patients with SI joint pain, especially those who experience it after a spinal fusion. Multiple published studies have documented the benefits of this procedure. Nationally, fully 95 percent of patients say they’d do it again. In my own practice, I’ve seen dramatic results when debilitating pain is reduced.
 Dr. John W. Aldridge is a Board certified orthopaedic surgeon with Hampton Roads Orthopaedic & Spine Center who has been specializing in minimally invasive muscle sparing spinal surgery and total joint replacement surgery in the Hampton Roads area since 2002. www.hrosm.com
Dr. John W. Aldridge is a Board certified orthopaedic surgeon with Hampton Roads Orthopaedic & Spine Center who has been specializing in minimally invasive muscle sparing spinal surgery and total joint replacement surgery in the Hampton Roads area since 2002. www.hrosm.com

