
A multidisciplinary program focusing on complex conditions of the brain and spine.
The relationship between the brain and spine is undeniably one of the most delicate and complex in the human body. The smallest misalignment in the spine or misfire in the brain – unless identified and treated by the most well trained and highly skilled neurosurgeon – can cause excruciating pain, debilitating loss of function and even death.
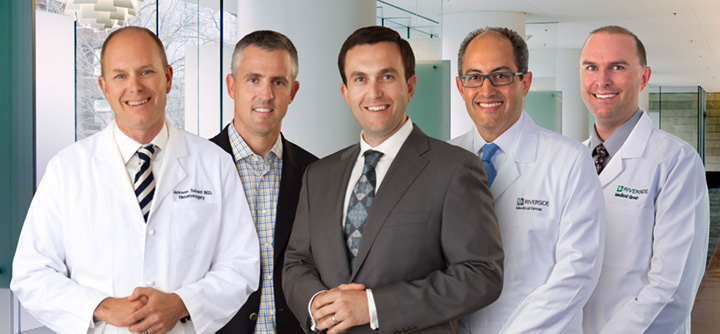
The surgeons of Riverside’s Neurological and Spine Institute have the knowledge, training and skill to treat these potentially devastating conditions with exquisite precision. Their combined years of surgical experience and mastery of 21st century technologies prove once again that Riverside Health System is providing the highest level of health care to the people of the Virginia Peninsula and beyond.
Despite their surgical expertise, these five neurosurgeons agree that surgery should always be the last resort. “Our job is to try to keep patients out of the operating room,” says Dr. Dean B. Kostov, “so that by the time the patient and I decide together to proceed with surgery, we know there’s nothing else that could have been done, and we know that the benefits will outweigh the risks.”
No surgery is without risk, but when conservative treatment fails or is inappropriate, or when patients no longer respond to medical therapies, surgery can be the correct choice. With the aid of the latest three-dimensional image guided, computer assisted navigation , these surgeons are able to perform complex and delicate, minimally invasive procedures for the most complicated cases, with results equivalent to those found in major university medical centers.
Unprecedented precision when micro-measurements count.
The use of a bi-plane digital x-ray in treating brain aneurysms is one example. Because in their earliest stages, aneurysms are asymptomatic, often the first sign of trouble is when they rupture. Between 30 and 50 percent of patients with a ruptured aneurysm die, or are left with significant disability; but when patients receive timely treatment, they can survive and even thrive.
Timely treatment used to mean craniotomy. Today, utilizing the bi-plane digital xray for guidance, Riverside surgeons insert a flexible catheter into the femoral artery, and thread it up through the neck into the brain; they can then insert a smaller catheter into the aneurysm through which progressively smaller platinum coils can be introduced until the aneurysm is tightly packed, thus depriving the aneurysm of its blood supply. The patient, headache and symptom free, goes home the next day.
The extraordinary high-resolution visualization of the brain’s vascular network made possible by the imaging technology is assisting surgeons in managing stroke cases as well.
Stereotactic radiosurgery – still the gold standard for brain tumors and abnormalities.
The concept of stereotactic radiosurgery, introduced in 1951 by Dr. Lars Leksell, has an impressive track record in treating brain tumors and other abnormalities. No other non-invasive treatment method in the field has greater clinical acceptance anywhere in the world. Riverside’s Neurological and Spine Institute employs two modalities that deliver stereotactic radiosurgery, both of which focus very high beams of radiation on a small part of the body.
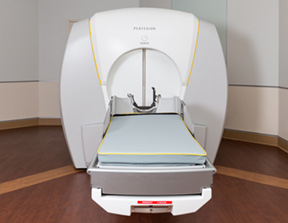
Gamma Knife – from the 4C to the Perfexion™
In 2015, after successfully utilizing the 4C model for nearly a decade, Riverside’s joint venture with University of Virginia and Chesapeake Regional acquired the latest iteration of the Gamma Knife: the Perfexion, then one of only 300 in the world.
The Gamma Knife delivers a single, finely focused, high dose of radiation to its target within the brain, causing little or no damage to surrounding tissue. The 4C allowed the surgeons to treat abnormalities measuring less than three centimeters, or one inch in diameter. The Perfexion system expands the treatable volume through an automated, multi-source collimator, and dramatically streamlines workflow. System benefits include faster set-up and treatment delivery to one or more tumors in a single session.
The Perfexion’s unique collimator is a permanent device divided into moveable sectors, ensuring superior conformity, accuracy and dosimetry while reducing residual dose to unintended areas. Integrated and intuitive treatment planning software facilitates creation of even the most complex plans (e.g., a donut-shaped dose distribution) by configuring composite shots that avoid overexposure to critical structures. Perfexion offers 98 percent reliability and unrivalled accuracy, guaranteed to 0.50mm.
“When the Gamma knife was invented, it was really meant to treat the center of the head, deep in the brain,” says Dr. William H. McAllister. “As it’s evolved, it’s become more of a primary modality for dealing with metastatic brain tumors. The problem with the design of the original unit was a lot of metastatic brain tumors occur right out on the periphery of the head, so if you had a tumor on the left and another on the right, with the old unit you could have a hard time getting to both of them: moving the head, you would actually bump into the actual machine and there would be an actual direct physical limitation as to how far you could move the patient to one side or the other in order to treat these tumors in multiple locations. The Perfexion was designed with that in mind.”
With years of experience behind them, Riverside surgeons are always finding ways to fine tune these procedures, making them more patient friendly. They have recently developed a new technique that allows them to preplan the treatment, using the patient’s diagnostic MRI. “We’re now able to do all the planning before the patient even comes to the Gamma Knife unit,” Dr. McAllister says. “where we used to have to put the head frame on the patient and sit at the computer for a half hour to plan, that’s no longer the case. The time the patient has to wait to begin the procedure is reduced, which in turn reduces anxiety.”
Further, with the Perfexion, the risks associated with open surgery are eliminated; because no incisions are required, the procedure can be performed using only local anesthesia. Treatment can be planned and programmed within a matter of an hour or two, requiring fewer MRI sequences. Treatment time is significantly less than conventional radiation and other delivery systems – often just one or two sessions – and because it’s most often done on an out-patient basis, most patients return to normal activity within 24-hours.

From Synergy-S to Varian – improved radiotherapy delivery.
For cancers of the spine (as well as neck, chest, lung, prostate, pancreas and liver) and for tumors in the brain not accessible to the Gamma Knife, Riverside neurosurgeons have had remarkable success with the Synergy-S delivery system, which combined a linear accelerator with an on-board CT scanner to visualize internal structures, including boney and soft tissues, in three dimensions prior to treatment.

However, advances in administering radiotherapy to these areas have enabled improvements in technologies, and Riverside has kept up, always seeking a safer, faster, more efficient delivery. The Neurological and Spine Institute is in the process of upgrading the Synergy-S to an entirely new and different system: as this is being written, the vault is being built to house the Varian EdgeTM system. The new Edge system has a real-time system architecture that enables a high level of synchronization between treatment planning, imaging, patient positioning, motion management, beam shaping, and dose delivery. The Edge will allow for tighter radiation dose gradients, resulting in better targeting and dose conformity of tumors with less radiation dose to normal tissues. Patient imaging and tumor tracking are also improved. The new upgraded Varian Edge system will continue to improve the success the neurosurgeons have seen over the past decade for intracranial and spine tumors.
Safer and more effective modalities to treat an aching back.
Among the reasons back surgery has such a negative reputation are the traditional methods of performing it. As open procedures, such operations required a long incision in the back that would allow the surgeon to cut down to the fascia and then peel away the muscles of the spine on both sides to expose the area needing surgical intervention. The unfortunate sequelae of open surgery were muscular damage and reduced circulation. Patient recovery was lengthy and exhausting.
“The challenge with any spine surgery is you’re trying to achieve two seemingly contradictory goals,” says Dr. Brian T. Farrell, the newest member of Riverside’s Neurological team. “You’re trying to decompress, and get the tissue out of the way of nerves that are pinched or disc material. And you have to do that in a way that preserves stability – so we’re always working on techniques that try to accomplish both.” He adds, “As a matter of our standard training, neurosurgeons spend a minimum of seven years learning and performing spine surgeries – including surgeries of the lumbar, cervical and thoracic spine.”
No matter how complicated the procedure nor how well trained the surgeon, precision is absolutely critical to a safe and effective result when operating on the spine. In today’s minimally invasive spine surgery, Riverside neurosurgeons localize the target area with intraoperative x-rays, allowing them to insert a dilator, a small tube that gently nudges the muscle fibers out of their way. Riverside Neurological and Spine Institute remains the only facility on the Peninsula with the capability to use both fluoroscopic and CT-based images intraoperatively. This capability, known as StealthStation, is a computer program that allows surgeons to build and visualize a 3-D model based on images obtained either from intraoperative x-rays obtained from a C-arm, or when indicated by the complexity of the pathology being treated, by intraoperative CT scans obtained from the O-arm. Because these 3-D images are more accurate than the traditional two-dimensional x-ray, the result is a quicker and more accurate operation.
“The O-arm and StealthStation work together; they’re intimately linked,” says Dr. Javier Amadeo. “They allow us to navigate instruments, very precisely, particularly for placing screws and rods in the spine.”
Minimally invasive spinal fusions.
For example, Dr. Amadeo explains, this technology allows him to perform procedures like the midline interbody lumbar fusion – Midlif, for short – with greater ease and precision: “When we do these fusions, we use something called pedicle screws that very securely anchor one vertebra to another vertebra through an intervening rod,” he says. “These screws have to be put in very precisely through the pedicle, a relatively narrow tubular structure that links the front part of the spine to the posterior. When you can thread a robust screw through there and into the front part of the spine, it’s a good way of providing fixation.”
He continues: “Doing this the traditional way, where the screw head is further out laterally and the tip of the screw points inward, we had to make a long incision and dissect the tissues out quite a bit laterally, about three and a half centimeters. In a Midlif, instead of using a lateral starting point, we start closer to the midline and angle the screw outward, thus we don’t have the same anatomical landmarks that we traditionally use that kind of give us a tactile feel for where the screw is going. The way we can do that by StealthStation guidance linked to the O-arm: that is, we get an O-arm set of images that are downloaded to the Stealth computer and the Stealth gives us a virtual image of the spine and a virtual image of the screw, and the drill we use to create the pilot hole. We know exactly where that screw is going, so it’s a novel technique for doing a standard traditional procedure in a less invasive way.”

Deep brain stimulation and movement disorders.
Many of the conditions that affect the nervous system are relatively free of observable symptoms, while others produce unmistakable signs of the disease within. Two such conditions are essential tremor and Parkinson’s disease. And because the symptoms are so similar and so overtly recognizable, many people believe they’re the same condition.
But despite their seemingly similar manifestations, they are in fact very different, notes Dr. Jackson B. Salvant, a neurosurgeon who works with these patients. No matter the etiology of the condition, patients with these conditions tend to suffer social anxiety, which especially in the case of essential tremor can exacerbate symptoms. While there is no cure for either condition, there are treatment options and techniques that can greatly improve the qualify of life of these patients.
Riverside has the only facility on the Peninsula that offers a unique treatment option to patients with either condition, Dr. Salvant says: “Deep brain stimulation, a modality that has shown significant results in controlling tremors. Prior to administering the stimulation, we give the patient mild sedation, and then under local anesthesia, we fit the patient with a frame similar to the Leksell frame used in Gamma Knife procedures. Once the frame is secure, the patient is awake, alert and responding to commands – so I’m able to test and measure the effects of the stimulation.”
Using MRI imaging and stereotactic techniques, the surgeon guides an electrical stimulation lead to a target deep within the brain in the area of the thalamus. The target areas for Essential Tremor and Parkinson’s are in relatively close proximity within the brain, but they are decidedly different in their functions and in the effects of treatment. Thus precision in reaching the appropriate target is critical.
Once a stimulating lead is precisely placed to obtain the ideal results, it is later connected to an implanted pulse generator similar to a pacemaker. The device then transmits painless electrical pulses to interrupt signals from the thalamus that may cause the tremors.
Awake brain tumor surgery with brain mapping.
Dr. Salvant also offers a unique surgical intervention for patients who have difficult brain tumors in locations where, if those patients were under general anesthesia, there is a higher potential for new neurological problems. “By doing the surgery with the patient awake and mapping the surface of the brain during surgery,” he says, “we can choose the safest avenue to perform the procedure, while getting real time monitoring of the patient’s condition. It allows us to avoid new neurological problems ensuing from the surgery.”
The awake procedure is highly effective, Dr. Salvant continues, but cautions: “We have to be very careful about who we offer that option to, because there are patients who are confused or disoriented, or who might have some underlying medical condition, like severe anxiety, for whom the procedure would not be appropriate. Even a significant fear of needles, or a history of poor interactions with a member of the medical community, could preclude some patients.”
Patient selection.
Just as critical to outcomes is the art of patient selection. Not every Neurological procedure is indicated for every patient with symptoms. The Riverside neurosurgeons, working with their colleagues at Riverside Neurological & Spine Institute – neurologists, neurovascular experts and neuroradiologists – insist on reserving the specialized treatment options considered herein for only those patients who will benefit the most. Each case is thoughtfully reviewed, and each procedure performed under the strictest criteria, done in coordination with other specialists.
Riverside Neurological and Spine Institute surgeons pride themselves on doing the right surgery at the right time for the right patient, says Dr. Farrell, and by carefully managing expectations. “We maintain a high standard as far as knowing when, and for whom, to recommend surgery.” As he counsels his patients, Dr. Kostov tells them, “We don’t operate on pictures; we operate on patients.”
What lies ahead.
“We’ve continued to evolve,” Dr. Kostov says. “We’ve pushed the technology and used it to make procedures safer. We’re utilizing robots more and more, and three-dimensional images acquired intraoperatively to tailor each procedure to each patient’s pathology.”
As for the future, he says, “Neurosurgery has always been on the cutting edge, because our imaging has always been improving, and we’re pushing it to be even better. We’re able to see tumors and nerve fibers better and better. What’s exciting about neurosurgery is that there’s always something new on the horizon that allows us to preserve neurological function while treating our patients for back and spine problems.”

